- Fact Checked
- December 05, 2025
- 20 min read
Mycoplasma Hominis: The Complete Guide to Understanding This Sneaky Bacteria
Table of Contents
Table of Contents
You know that friend who walks into a situation, stirs up just enough drama to cause chaos, then swears they had nothing to do with it? That’s Mycoplasma hominis.
Most of the time, it’s a harmless bacterium in your body’s natural flora, quietly minding its own business. But when the balance shifts—maybe your immune system is stressed, your good bacteria take a hit, or your vaginal pH changes—it can start trouble fast.
At Happy V, we believe that understanding bacteria like M. hominis is the first step to keeping your microbiome balanced, your confidence high, and the drama out of your vaginal health.
This post is for informational purposes only and does not constitute medical advice. See full disclaimer below.
What Is Mycoplasma hominis?
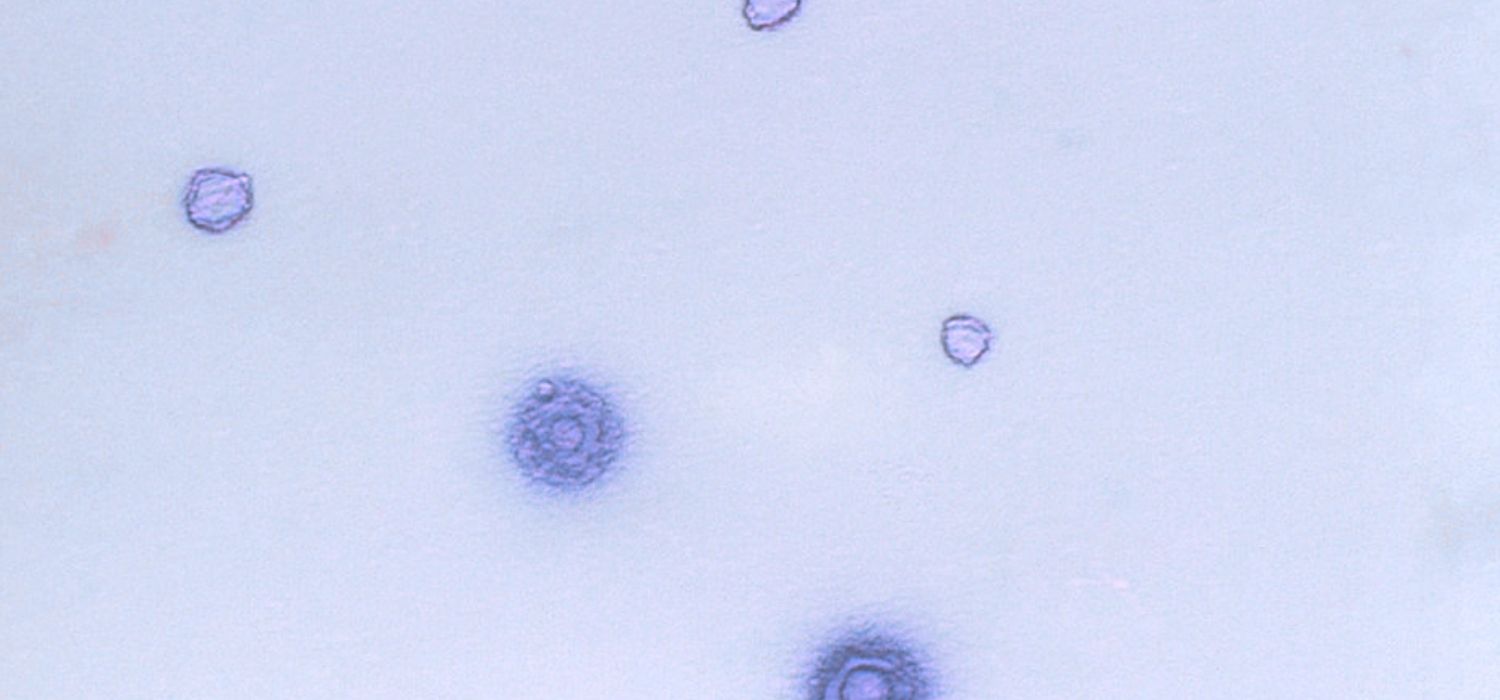
Mycoplasma hominis, or M. hominis, belongs to a unique family of bacteria that's quite honestly pretty fascinating… at least from a microbiology standpoint1.
Unlike the bacteria you might be more familiar with (think: Gardnerella vaginalis or E. coli), M. hominis doesn't have a cell wall. This might sound like a minor detail, but it's actually huge! It's what makes this bacteria both harder to detect and trickier to treat.
The Cell Wall Mystery
Most bacteria are surrounded by a rigid cell wall that gives them structure and protection2. It's like their armor. M. hominis? It's essentially going through life naked, surrounded only by a flexible cell membrane. This makes it incredibly small (among the smallest free-living microorganisms on Earth, actually) and gives it a unique ability to squeeze through tiny spaces and change shape.
This lack of a cell wall also explains why many common antibiotics don't work against it. Antibiotics like penicillin work by attacking bacterial cell walls, so when there's no wall to attack, the antibiotic is essentially useless. This is why tetracycline antibiotics like doxycycline or macrolides like azithromycin are typically needed for M. hominis infections.
Where Does It Live?
Mycoplasma hominis has a particular fondness for the urogenital tract, or the urinary and reproductive systems3. In women, it's commonly found in the vagina, cervical area, and sometimes the upper reproductive tract. In men, it typically hangs out in the urethra and can sometimes contribute to urethritis or prostatitis.
Research shows that M. hominis can be detected in about 15-20% of sexually active individuals, though this number varies significantly based on factors like age, sexual activity, and overall health status4. What's important to understand is that many of these people have zero symptoms. The bacteria is just quietly living there as part of their normal genital tract flora.
When It’s Harmless vs. Harmful:
M. hominis is generally harmless when kept in check by a healthy vaginal microbiome rich in protective Lactobacillus species5. In these cases, it lives quietly without causing inflammation or symptoms. It becomes harmful when that balance is disrupted by things like antibiotics, hormonal changes, immune suppression, or other infections, allowing it to overgrow and potentially cause conditions like bacterial vaginosis (BV), pelvic inflammatory disease (PID), postpartum infections, or complications during pregnancy.
The Mycoplasma Species Family
M. hominis isn't the only member of its bacterial family that can affect the genital tract. Other important mycoplasma species include:
Mycoplasma genitalium (M. genitalium): This species is more clearly associated with urethritis and is more likely to be considered a true sexually transmitted infection (STI) requiring treatment when detected. M. genitalium is often more problematic than M. hominis6 and has been linked to serious complications, including pelvic inflammatory disease (PID).
Ureaplasma species: These include Ureaplasma urealyticum and other ureaplasma species that can also colonize the urogenital tract. Like M. hominis, ureaplasma can exist harmlessly but may cause problems under certain conditions7. The relationship between these genital mycoplasma organisms means that healthcare providers often test for multiple species simultaneously.
Understanding these distinctions is important because testing often screens for multiple mycoplasma bacteria simultaneously, and treatment approaches may differ depending on which organisms are detected.
The Link Between M. hominis and Vaginal Health
Your vaginal microbiome is like a self-sustaining ecosystem, with friendly Lactobacillus bacteria acting as its security team8. When this team is strong, M. hominis can coexist peacefully without causing trouble. But when protective lactobacilli are depleted, whether from antibiotics, hormonal shifts, stress, unprotected sex, or other infections, the environment becomes less acidic and more welcoming to opportunistic bacteria like M. hominis.
Prebiotic + Probiotic
Maintains vaginal pH and restores gut health.
In this disrupted state, M. hominis can multiply and tip the balance further toward dysbiosis, sometimes triggering or contributing to conditions like bacterial vaginosis (BV), postpartum infections, or pelvic inflammatory disease (PID)9. It’s also been found more frequently in women with recurrent BV, suggesting that once the microbiome is destabilized, M. hominis may help sustain the imbalance.
Does M. hominis Cause BV?
M. hominis isn’t considered the primary cause of bacterial vaginosis (that role is more often linked to bacteria like Gardnerella vaginalis). However, research shows M. hominis is frequently found in higher numbers in women with BV compared to those with a healthy vaginal microbiome10.
This suggests that M. hominis may not start the BV process, but it can thrive in the altered environment BV creates. Once it multiplies, it can contribute to ongoing symptoms and make it harder for the microbiome to return to a balanced, lactobacillus-dominant state.
In other words: BV can open the door, and M. hominis can take advantage of the invitation and continue to take space and resources away from healthy, protective bacteria, like Lactobacillus.
Causes and Risk Factors
Understanding your risk factors isn't about blame or judgment. It's about empowerment. When you know what conditions can make M. hominis more likely to become a pathogen rather than a harmless colonizer, you can take proactive steps to protect yourself.
1. Vaginal Microbiome Disruption and Bacterial Vaginosis
Your vaginal microbiome is like a protective security system, and Lactobacillus bacteria are the elite guards11. These beneficial bacteria produce lactic acid and hydrogen peroxide, creating an acidic environment (typically pH 3.8-4.5) that most harmful microorganisms can't survive in.
When Lactobacillus levels drop, whether due to antibiotics, douching, hormonal changes, or other factors, the vaginal pH rises, creating a more hospitable environment for organisms like M. hominis to flourish12. This is why bacterial vaginosis and M. hominis infections sometimes occur together. In fact, epidemiological studies have shown that bacterial vaginosis creates conditions that can allow various bacterial infections to take hold.
Research published in multiple studies demonstrates the strong connection between bacterial vaginosis and mycoplasma hominis colonization, particularly when the normal vaginal microbiome is disrupted13.
2. Sexual Activity and STI Considerations
While M. hominis isn't classified as a traditional sexually transmitted infection like chlamydia trachomatis, sexual activity can influence its presence and behavior14. Each sexual partner introduces their unique microbial community, and sometimes this mixing of microbiomes can tip the balance.
Multiple sexual partners or new sexual relationships can increase exposure to different bacterial communities. It's not that any particular bacteria is inherently "bad"—it's that your body needs time to adjust to new microbial influences. This is why M. hominis is sometimes grouped with other STD/STI testing panels, even though it doesn't meet the strict definition of a traditional sexually transmitted infection15.
3. Antibiotic Use and Microbiome Recovery
Antibiotics are incredibly powerful tools that save lives, but they're also pretty much a bacterial bomb16. While eliminating the harmful bacteria causing your infection, they often take out beneficial bacteria too. This creates what microbiome researchers call "colonization resistance.” Essentially, when your protective bacteria are depleted, opportunistic organisms have space to move in and potentially cause problems.
This is particularly relevant with broad-spectrum antibiotics, which affect a wide range of bacterial species17. The recovery period after antibiotic treatment is a crucial window where supporting your microbiome with targeted probiotics becomes especially important for preventing M. hominis infections.
4. Immune System Factors and Immunocompromised Patients
Your immune system works closely with your microbiome to maintain health18. When immune function is compromised due to stress, illness, poor nutrition, lack of sleep, or medical conditions, your body's ability to keep potentially problematic bacteria in check can be reduced.
This is particularly important for immunocompromised patients, who may be more susceptible to M. hominis infections and may experience more severe symptoms. Research in infectious diseases has shown that individuals with weakened immune systems may need more aggressive treatment approaches for mycoplasma bacteria and are at higher risk for complications.
Symptoms of Mycoplasma Hominis
One of the most frustrating things about M. hominis is that it's a master of disguise. Many people who carry it have absolutely no symptoms, while others experience issues that can easily be mistaken for other common conditions.
The Asymptomatic Majority
Research suggests that the majority of people who carry M. hominis experience no symptoms at all. This isn't necessarily a bad thing. It often means your body's natural defense systems are working effectively to keep everything in balance.
However, this also means that routine testing becomes more important if you're experiencing recurrent vaginal health issues or if your healthcare provider suspects an underlying infection that's been difficult to identify through standard STI screening19.
When Symptoms Do Appear
When M. hominis does cause symptoms, they tend to be relatively subtle and can easily overlap with other conditions20. Common issues include:
- Vaginal discharge changes: This might be an increase in vaginal discharge, a change in color (often grayish or yellowish), or a change in odor. Unlike the classic "fishy" smell associated with bacterial vaginosis, M. hominis might produce a more subtle, musty odor.
- Pelvic discomfort: This can range from a dull ache to more noticeable pain, particularly in the lower abdomen or pelvis. Some people describe it as feeling "heavy" or "full" in the pelvic area.
- Urinary tract symptoms: Burning during urination, increased frequency, or urgency can occur, though these symptoms are more commonly associated with traditional urinary tract infections.
- Sexual discomfort: Pain during penetration or general discomfort during sexual activity can be a sign that something's off with your genital tract health.
- Systemic symptoms: In some cases, particularly if the infection spreads to the upper reproductive tract and causes pelvic inflammatory disease (PID), you might experience low-grade fever, fatigue, or general malaise.
The Overlap Challenge and Differential Diagnosis
The tricky thing about these symptoms is that they're shared with many other conditions, including bacterial vaginosis, yeast infections, urinary tract infections, and various STIs can all cause similar issues. This is why self-diagnosis is rarely accurate and why proper testing, often including PCR (polymerase chain reaction) methods, becomes so important21.
Healthcare providers often need to consider multiple possibilities when evaluating urogenital symptoms, including other mycoplasma species, ureaplasma species, and more common pathogens to ensure accurate diagnosis and appropriate treatment22.
The Testing Process: What to Expect and How to Prepare
Getting tested for M. hominis has become much more straightforward in recent years, thanks to advances in molecular diagnostic techniques. Understanding what to expect can help reduce anxiety and ensure you get the most accurate results.
Modern PCR Testing Methods
Gone are the days when mycoplasma testing required complex culture methods that could take weeks to yield results. Today's molecular testing—which is primarily polymerase chain reaction (PCR)—can detect bacterial DNA quickly and accurately23.
PCR testing is incredibly sensitive, meaning it can detect very small amounts of bacterial genetic material24. This is generally a good thing, but it also means that a positive result doesn't automatically indicate an active infection requiring treatment. Many laboratories now use multiplex PCR panels that can simultaneously test for M. hominis, M. genitalium, ureaplasma species, and other common urogenital pathogens.
Sample Collection: The Reality
There are several ways your doctor may collect a sample for testing. These are relatively quick and painless and can include:
- Vaginal testing: Your healthcare provider will use a sterile swab to collect a sample from your vagina. The process is similar to a Pap smear It might feel slightly uncomfortable or awkward, but it's typically quick (usually under 30 seconds). Some providers can also use self-collected vaginal swabs, which many people find more comfortable.
- Urine testing: This involves providing a urine sample, typically the "first catch" of your morning urine or the first part of your urine stream. This method is completely non-invasive and can be just as accurate as vaginal swabs for detecting genital mycoplasma.
- Cervical testing: In some cases, particularly if there are concerns about upper reproductive tract involvement, your provider might collect a cervical sample during a pelvic examination.
Timing Considerations
The timing of your test can affect results. If you're menstruating, some providers prefer to wait until after your period, as menstrual blood can sometimes interfere with testing. However, this isn't always necessary with modern PCR methods.
If you've recently taken antibiotics, this could affect test results, too. Generally, it's recommended to wait at least 2-4 weeks after completing antibiotic treatment before testing, unless you're experiencing active symptoms that need immediate attention.
Results Timeline and What They Mean
Most molecular tests for M. hominis return results within 1-3 days, though this can vary depending on your healthcare provider and laboratory.
A positive result of M. hominis DNA confirms the bacteria is present but doesn't automatically mean you have an infection requiring treatment. A negative result generally means the bacteria isn't present in detectable amounts.
Some tests also provide information about the amount of bacteria detected, which can help your provider determine whether treatment is likely to be beneficial.
Interpreting Test Results: The Art and Science of Diagnosis
This is where things get nuanced, and why having a knowledgeable healthcare provider is so important. A positive test for M. hominis doesn't automatically mean you need treatment25. It depends on if you are dealing with colonization or infection.
The Colonizer vs. Pathogen Distinction
M. hominis can exist in two states: as a harmless colonizer (just living there peacefully) or as a pathogen (actively causing problems). The same bacteria can be completely benign in one person while causing symptoms in another, or even be harmless in the same person at one time and problematic at another.
Your healthcare provider will consider several factors when interpreting a positive result:
- Symptom correlation: Are your symptoms consistent with M. hominis infections? Do they fit the timeline of when you might have been exposed?
- Bacterial load: Some tests can quantify how much bacteria is present. Higher amounts are more likely to be clinically significant.
- Co-infections: Is M. hominis present along with other bacteria that are known to cause problems? Sometimes bacterial infections work in combination to cause symptoms.
- Your health history: Do you have recurrent vaginal infections? Are you immunocompromised? Have you had pelvic inflammatory disease before?
- Response to previous treatments: Have you been treated for other vaginal infections recently, and did those treatments help?
Treatment Approaches: Beyond Just Antibiotics
Because M. hominis lacks a cell wall, treatment requires specific antibiotics that work through different mechanisms than the penicillin-type antibiotics many people are familiar with.
First-Line Treatment Options
If you are prescribed antibiotics for symptomatic M. hominis overgrowth, these most often include:
- Doxycycline: This tetracycline antibiotic is often the first choice because it effectively penetrates cells and works well against mycoplasma species. It's typically prescribed for 7-14 days, and it's important to take it with food to reduce stomach upset and avoid dairy products or calcium supplements within a few hours of taking it.
- Azithromycin: This macrolide antibiotic is another excellent choice, particularly for people who can't tolerate doxycycline. It has the advantage of a shorter treatment course (often just 1-5 days) and fewer dietary restrictions. Azithromycin is also effective against other mycoplasma species and ureaplasma species.
- Clindamycin: This antibiotic can be effective against M. hominis and is sometimes used when other options aren't suitable. It can be taken orally or, in some cases, used as a vaginal cream or suppository.
The choice between these antibiotics often depends on patient factors, resistance patterns in your geographic area, and whether other mycoplasma bacteria or ureaplasma species are also present.
Special Considerations for Treatment
Aside from which antibiotic to take, an antibiotic prescription comes with more considerations, like:
- Resistance patterns: Like other bacteria, M. hominis can develop resistance to antibiotics. Some strains have shown resistance to certain macrolides, which is why sensitivity testing may be recommended in cases of treatment failure. This is an area of active research in microbiology, with new resistance patterns emerging regularly.
- Partner treatment: Depending on your situation and whether M. hominis is considered the likely cause of your symptoms, your healthcare provider might recommend that your sexual partner(s) also be tested or treated to prevent reinfection.
- Pregnancy considerations: Treatment approaches may need to be modified for pregnant individuals, as some antibiotics commonly used for M. hominis may not be safe during pregnancy.
Treatment for Related Conditions
Since M. hominis infections often occur alongside other conditions, comprehensive treatment may be needed. Common coinfections/treatments include:
- Bacterial vaginosis treatment: If BV is present alongside M. hominis, treating both conditions simultaneously may improve outcomes and reduce recurrence rates.
- PID treatment: If M. hominis has contributed to pelvic inflammatory disease, more aggressive antibiotic treatment may be needed, sometimes requiring hospitalization for intravenous antibiotics.
- Urinary tract involvement: If M. hominis is affecting the urinary tract, treatment duration may be extended and specific antibiotics that concentrate well in urinary tissues may be preferred.
Prevention Strategies: Building Long-Term Vaginal Health
The best approach to dealing with M. hominis (and vaginal health issues in general) is prevention. This doesn't mean you can prevent every possible issue, but you can definitely stack the odds in your favor.
Targeted Microbiome Support
The stronger and more balanced your vaginal microbiome is, the better it can protect you from opportunistic bacterial infections. One of the best ways to help maintain that balance is through targeted vaginal probiotics.
Not all probiotics are created equal, though—strain specificity matters. You want products containing Lactobacillus strains that have been researched specifically for vaginal health. Happy V’s Prebiotic + Probiotic, for example, includes Lactobacillus acidophilus LA14 and Lactobacillus rhamnosus HN001, two clinically studied strains shown to work synergistically.
LA14 has been studied for its ability to colonize the vaginal tract, produce lactic acid, and help maintain an acidic pH that makes it harder for opportunistic bacteria to overgrow. HN001, meanwhile, supports both vaginal and immune health, with research suggesting it can help modulate inflammation and improve resilience against dysbiosis. When taken together, these strains can help reinforce the protective lactobacillus population, stabilize pH, and create a less hospitable environment for bacteria like M. hominis.
The result? A microbiome that’s better equipped to defend itself naturally—without waiting for symptoms to appear.
Consistency matters: Supporting your microbiome isn't a one-time thing. It's an ongoing process. Regular probiotic supplementation can be particularly important during times of stress, illness, or antibiotic use when your natural bacterial balance might be more vulnerable to disruption.
Smart Sexual Health Practices
As you might imagine, vaginal health and sexual health are linked. To prevent infections and the uncomfortable symptoms that come with them:
- Communicate with partners: Open, honest communication about sexual health isn't just good relationship practice—it's good health practice. This includes discussing recent STI testing, any symptoms, and sexual history, particularly given that mycoplasma bacteria can be transmitted between partners.
- Use barrier protection: Condoms and dental dams don't just protect against traditional STIs—they can also help maintain microbial balance by reducing the exchange of bacteria between partners.
- Have good post-sex hygiene: Urinating after sexual activity can help flush out any bacteria that might have been introduced to the urinary tract. Gentle external cleansing with water is fine, but avoid douching or using harsh soaps internally.
Potential Complications of M. hominis
While M. hominis often exists harmlessly in the genital tract, certain situations can turn it from a quiet bystander into a genuine health concern. In these cases, the stakes are higher, and prompt recognition is essential.
Pregnancy and Neonatal Risks
During pregnancy, M. hominis can pose risks that go beyond maternal discomfort:
- Chorioamnionitis – This infection of the fetal membranes has been linked to M. hominis and can lead to preterm labor, premature rupture of membranes, and other complications requiring urgent treatment26.
- Neonatal Infections – In rare instances, M. hominis can pass from mother to baby during delivery, potentially affecting the newborn’s respiratory, joint, or central nervous systems27. Severe outcomes are uncommon but possible.
- Treatment Challenges – Some of the most effective antibiotics for M. hominis aren’t recommended during pregnancy, so providers must carefully choose options that balance maternal and fetal safety.
High-Risk Populations
People with weakened immune systems—whether due to chronic illness, medications, or other factors—are more vulnerable to symptomatic and persistent infections:
- Greater Susceptibility – A reduced immune defense makes it easier for M. hominis to overgrow and cause prolonged symptoms.
- Longer or Complex Treatments – Clearing the infection may require extended antibiotic courses or combination therapies.
- Close Monitoring – Frequent follow-up testing helps ensure the infection has cleared and detects any recurrence early.
Related and Co-Occurring Infections
M. hominis rarely operates alone in the urogenital tract:
- Other Genital Mycoplasmas – Co-infections with M. genitalium or Ureaplasma species are common and may influence symptoms, treatment choice, and recurrence risk28.
- Broader Mycoplasma Context – While M. pneumoniae is a respiratory pathogen, it’s a reminder that mycoplasmas as a group can cause infections in multiple body systems—highlighting their adaptability and clinical complexity29.
Frequently Asked Questions
Is M. hominis the same as other mycoplasma species?
No. While related, M. hominis is distinct from species like M. genitalium and Ureaplasma, which differ in clinical significance and treatment approaches.
Can M. hominis affect fertility or cause PID?
Rarely, but if it contributes to PID or upper reproductive tract infections, it could impact fertility, which is why persistent symptoms should be evaluated.
How accurate is PCR testing for M. hominis?
PCR is highly accurate at detecting M. hominis DNA, but a positive result doesn’t always mean you have an active infection since it can exist in normal, balanced floras.
Should my partner be tested if I have M. hominis?
It depends on your symptoms and provider’s assessment, as partner testing isn’t always needed for M. hominis unlike typical STIs.
Can probiotics prevent M. hominis infections?
Nothing is a guarantee, but doctor-formulated vaginal probiotics can help maintain a vaginal environment less favorable to infection.
What's the difference between M. hominis and a traditional STD?
Unlike classic STDs, M. hominis can be found in people who aren’t sexually active and isn’t always harmful, though it can be sexually transmitted.
Can M. hominis cause chronic symptoms?
Sometimes, but chronic pelvic or vaginal issues usually have multiple causes and may require specialist evaluation.
How long does treatment take to work?
Antibiotics typically work within 7–14 days, though full microbiome recovery can take weeks to months.
Are there any natural treatments for M. hominis?
For active infections, antibiotics are needed, but probiotics and healthy habits support recovery and prevention.
What should I do if symptoms return after treatment?
Check back in with your healthcare provider for another test and to see if a different antibiotic might help. Sometimes symptoms return because the bacteria is resistant or you’ve been reinfected.
Final Thoughts
Understanding M. hominis is really about seeing the bigger picture of vaginal health. It’s a reminder that the presence of a microorganism doesn’t always mean infection, and that your vaginal ecosystem thrives on balance.
The empowering part? You have control over many factors that influence that balance, from probiotics and sexual health practices to stress management and antibiotic use. At Happy V, we believe that supporting your microbiome is one of the best investments you can make in your long-term wellness.
Keep the Conversation Going
- Visit our blog for more women's health tips.
- Join our private Happy V Facebook group to hear from others who've been there.
- Explore supplements designed to support your vaginal health journey.
Disclaimer: This blog is for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Statements about supplements have not been evaluated by the Food and Drug Administration. For more information about vaginal infections, visit the CDC or speak to a licensed healthcare provider.















