- Fact Checked
- December 11, 2025
- 18 min read
Cytolytic Vaginosis: The Overlooked Cause of Vaginal Discomfort
Table of Contents
Table of Contents
So you're dealing with itching, burning, and that thick, white vaginal discharge. It must be a yeast infection, right? But here's the plot twist: your tests for Candida come back negative. So do your tests for Gardnerella… and Trichomonas. What's going on?
If you are experiencing symptoms of yeast infection without the yeast, you might be experiencing cytolytic vaginosis, a condition that's way more common than most people realize but rarely gets the spotlight it deserves outside of specialized gynecology or obstetrics practices.
This lack of awareness means many folks end up on a frustrating merry-go-round of unnecessary antifungal treatments or antibiotics that can actually make symptoms worse. We’re here to change that, with a deep dive into how cytolytic vaginosis happens, why it’s so often mistaken for other vaginal conditions, and (most importantly) what you can do to get relief and keep it from coming back.
This post is for informational purposes only and does not constitute medical advice. See full disclaimer below.
What is Cytolytic Vaginosis (CV)?
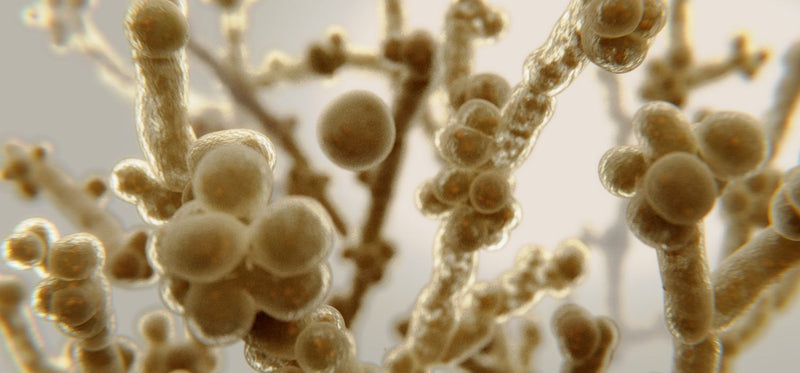
In a healthy vaginal environment, your lactobacilli (including superstars like Lactobacillus crispatus and L. acidophilus) are kind of like your personal bodyguards. They work hard to maintain your vaginal health by producing lactic acid and sometimes hydrogen peroxide, keeping your vaginal pH in that sweet spot of 3.5–4.5. This creates a protective barrier against troublemakers like Candida and Gardnerella (the #1 culprits behind yeast infections and BV, respectively).
In cytolytic vaginosis, these well-meaning lactobacilli become a bit overzealous1. Their numbers shoot up abnormally high, creating excessive acidity. This extra acidity actually damages your vaginal epithelial cells, releasing glycogen and triggering a breakdown process that scientists call Doderlein's cytolysis.
The result? Irritation, discomfort, and symptoms that look almost identical to other vaginal infections, but require a completely different approach to treatment.
Symptoms of Cytolytic Vaginosis
The symptoms of cytolytic vaginosis can feel frustratingly familiar if you’ve dealt with other vaginal conditions before:
- Pruritus (itching) or a burning sensation around your vulva
- Thick, white, odorless vaginal discharge
- Dyspareunia, or discomfort during intercourse
- Dysuria, or that super uncomfortable burning feeling when you pee, commonly associated with urinary tract infections (UTIs)
Studies show that symptoms of CV often flare during the luteal phase of your menstrual cycle (or the time between ovulation and the start of your next period), when hormone levels like estrogen and progesterone rise, increasing glycogen in the vaginal lining2. This glycogen becomes food for lactobacilli, allowing them to multiply quickly and push vaginal acidity higher.
What Cytolytic Vaginosis Is Often Confused With
Because the symptoms of cytolytic vaginosis often mirror those of other common vaginal infections, it often gets misdiagnosed for conditions like:
Vulvovaginal candidiasis (yeast infection) – Thick, white discharge and itching are very similar to CV, but yeast infections involve fungal overgrowth, while CV does not3.
Bacterial vaginosis – Like CV, BV usually presents with a higher vaginal pH, but it usually also involves a noticeable fishy odor, which CV does not4.
Trichomoniasis – This sexually transmitted infection can cause similar itching and discharge but is often accompanied by frothy, yellow-green fluid and will test positive for Trichomonas5.
Non-infectious vaginitis – Irritant or allergic reactions can mimic burning and redness without altering the balance of the vaginal flora6.
Without proper testing, and especially that all-important wet mount microscopy (which we’ll get into later), these vaginal conditions can be frustratingly difficult to tell apart, leading to treatment options that just don't hit the mark and leave you uncomfortable.
Cytolytic Vaginosis vs. Other Common Vaginal Infections
Because cytolytic vaginosis shares symptoms with several other vaginal conditions, it’s important to understand the key differences. The table below compares CV with yeast infections, bacterial vaginosis, and trichomoniasis in terms of cause, symptoms, and treatment.
| Feature | Cytolytic Vaginosis (CV) | Yeast Infection (Vulvovaginal Candidiasis) | Bacterial Vaginosis (BV) | Trichomoniasis |
| Main Cause | Overgrowth of lactobacilli causing overly acidic vaginal pH | Overgrowth of Candida fungus | Overgrowth of anaerobic bacteria (e.g., gardnerella) | Infection with Trichomonas vaginalis parasite |
| Vaginal pH | Low (3.5–4.5) | Normal to slightly acidic (~4.0–4.5) | High (>4.5) | High (>4.5) |
| Discharge | Thick, white, odorless | Thick, white, "cottage cheese–like" | Thin, gray/white with fishy odor | Frothy, yellow-green, often with strong odor |
| Odor | None | None | Fishy | Foul or musty |
| Itching / Burning | Common, may worsen in luteal phase | Common, intense | Mild or absent | Common, often with redness/swelling |
| Pain During Sex (Dyspareunia) | Sometimes | Sometimes | Occasionally | Often |
| Burning with Urination (Dysuria) | Sometimes | Sometimes | Rare | Often |
| Key Microscopy Findings | Abundant lactobacilli, lysed epithelial cells, few white blood cells | Budding yeast or pseudohyphae | Clue cells, reduced lactobacilli | Motile trichomonads, many white blood cells |
| Responds to Antifungals? | No | Yes | No | No |
| Typical Treatment | Alkalinizing measures (baking soda sitz baths, avoiding pH-lowering products) | Antifungal cream or oral medication | Antibiotics (e.g., metronidazole | Antibiotics (metronidazole or tinidazole) |
| Contagious? | No | No | No | Yes – sexually transmitted |
Causes and Risk Factors
While your lactobacilli are generally the heroes of your vaginal health story, balance truly is everything. When these helpful bacteria multiply a bit too enthusiastically, your vaginal pH drops below the optimal range, creating an overly acidic environment that can irritate your vaginal epithelium. Several everyday factors can tip this delicate balance toward an overgrowth of lactobacilli, like:
Taking too Many Probiotics
Many probiotic blends are designed to boost your lactobacilli levels. While this is fantastic for conditions like bacterial vaginosis, in cytolytic vaginosis, this "more is better" approach actually pushes your lactobacilli into overdrive, making your vaginal environment too acidic for comfort (literally).
Frequent Douching or Harsh, Scented Cleansers
Despite what some marketing might suggest, douche solutions and perfumed washes can actually disrupt your natural vaginal flora by washing away the other helpful microorganisms that keep your lactobacilli in check. Once those balancing species get reduced, your lactobacilli can take over the neighborhood and cause that troublesome Doderlein's cytolysis.
Hormonal Fluctuations During Your Menstrual Cycle, Pregnancy, or From High-Estrogen Contraceptives
Estrogen is like rocket fuel for your vaginal epithelial cells, stimulating them to produce more glycogen7. Since lactobacilli absolutely love to feast on glycogen (converting it into lactic acid and lowering your vaginal pH), high-estrogen states basically set up an all-you-can-eat buffet that allows lactobacilli to multiply rapidly.
Extended Tampon Use or Tight Clothing
Tampons and snug-fitting, synthetic underwear create a cozy, trapped environment that's warm and moist, basically a luxury spa for microbial overgrowth. In cytolytic vaginosis, this microclimate becomes the perfect breeding ground for lactobacilli by maintaining that stable, warm, acidic environment they thrive in.
Overdoing Antifungal or Antibiotic Therapies for Presumed Vaginal Infections
Antifungal treatments (like those used to treat a presumed vaginal yeast infection) don't affect lactobacilli at all, but they can wipe out competing organisms like Candida, essentially removing a natural check on lactobacilli growth8. Similarly, antibiotics (like those used to treat UTIs and BV) can eliminate a wide range of bacteria, including the ones that help maintain balance in your vaginal microbiome, leaving your lactobacilli free to dominate the scene.
In each of these scenarios, the common theme is reduced microbial diversity combined with an increased food supply for lactobacilli. Both factors work together to allow their population to spike while your vaginal pH takes a nosedive, setting the stage for all that irritation, discharge, and discomfort that defines cytolytic vaginosis. So, essentially, the treatment used to treat a misdiagnosis can fuel the true cause of your discomfort.
CV Diagnosis & Testing
Since cytolytic vaginosis is such a convincing impersonator of yeast infections, bacterial vaginosis, and trichomoniasis, getting the right diagnosis is absolutely crucial. Treating the wrong condition doesn't just delay your relief; it can actually make your symptoms worse!
A knowledgeable women's health provider (think: someone in gynecology or obstetrics) will typically walk through these steps with you:
Detailed Medical History
They'll want to know about your symptom timeline, especially if things seem to flare up during the luteal phase of your menstrual cycle. They'll also ask about recent use of probiotics, douche products, antibiotics, or antifungal treatments, plus your history with vaginal infections and how they were treated.
Physical Exam
This involves a gentle inspection of your vulva and vaginal canal to check for redness, swelling, or irritation, plus an assessment of your discharge (cytolytic vaginosis typically produces that characteristic thick, white, odorless fluid).
Vaginal pH Test
This simple test is super telling! Cytolytic vaginosis usually shows up with a pH between 3.5–4.5, while BV or trich will reveal higher pH levels9.
Wet Mount Microscopy
This is where the magic happens. A tiny sample of your discharge gets examined under a microscope, and CV has a very distinctive signature. Under a microscope, CV looks like:
- Abundant lactobacilli everywhere10
- Lysed vaginal epithelial cells11
- Few or no white blood cells (unlike infections that trigger your immune system to send in reinforcements)
Ruling Out Other Conditions
If results aren't crystal clear, your provider might run specific tests for Candida, Gardnerella, and Trichomonas12. Sometimes a pap smear might incidentally reveal cytolysis, but it's not the go-to diagnostic tool for this condition.
Why microscopy is your best friend: Visual symptoms alone are notoriously unreliable for distinguishing cytolytic vaginosis from other vaginal conditions. Lab confirmation ensures your treatment plan will actually help restore harmony to your vaginal microbiome, rather than accidentally making things worse.
Who Should Be Tested for Cytolytic Vaginosis
You might want to have a conversation with your healthcare provider about CV testing if any of these sound familiar:
- You've been dealing with vaginal discharge, itching, or burning for more than a week, but your tests for candida, bacterial vaginosis, and trichomoniasis keep coming back negative13
- Your symptoms have a predictable pattern of getting worse during certain times in your menstrual cycle14
- Antifungal treatments haven't provided relief, or have actually made things feel worse15
- You've been faithfully using probiotics, boric acid, vitamin C, or pH-lowering "vaginal health" products without seeing improvement
- You've been stuck in a cycle of "yeast infection" diagnoses that never quite match your test results16
- You're tired of the trial-and-error approach and want to avoid repeated misdiagnosis and unnecessary antibiotics or antifungals17
Testing becomes especially valuable if you feel like you're caught in an endless loop of treatments that aren't working. The right diagnosis can break that frustrating cycle and get you back to feeling comfortable and confident.
Treatment Options
The beautiful thing about treating cytolytic vaginosis is that the goal is gentle and straightforward: calm that overgrowth of lactobacilli, give your vaginal pH a slight boost, and help restore a healthy microbial balance, all without nuking the beneficial bacteria you actually want to keep around.
Most people start feeling significantly better within 1-3 weeks when treatment is properly targeted.
Here are the most effective, evidence-backed treatment options that actually work:
1. Baking Soda (Sodium Bicarbonate) Sitz Baths
Sitz baths are probably the gentlest, most soothing way to help alkalinize your vaginal environment. Think of it as giving your irritated tissues a peaceful, healing spa treatment.
How to create your at-home spa experience:
- Fill your bathtub with 2–3 inches of warm water (just enough to comfortably cover your vulva and vaginal opening)
- Dissolve 2–4 tablespoons of baking soda into the water, stirring until it's completely dissolved
- Settle in and soak for a relaxing 15–20 minutes
- Start with 2–3 sessions during your first week, then dial it back to once or twice weekly as you feel better
Why this works so well: Baking soda gently raises your pH level, creating a less acidic environment where lactobacilli growth naturally slows down, and that uncomfortable irritation starts to fade.
2. Baking Soda Vaginal Suppository
These provide targeted, direct alkalinization right where you need it most—inside your vagina.
Your DIY approach:
- Fill empty gelatin capsules (size 00 works great) with baking soda
- Insert 1 capsule into your vagina twice weekly for 2 weeks
- Many people notice symptom relief within just a few days, but stick with the full course to maintain that healthy balance
Important note: Only try this after you've gotten a confirmed cytolytic vaginosis diagnosis. Overuse can swing your pH too far in the opposite direction and potentially trigger bacterial vaginosis or aerobic vaginitis.
3. Baking Soda Douche (only if your healthcare provider gives the green light!)
While we (and most healthcare providers) generally don't recommend routine douche use, short-term use specifically for cytolytic vaginosis can be helpful when done under medical guidance.
If your provider recommends this approach:
- Mix 1–2 tablespoons of baking soda with 4 cups of warm, distilled water
- Use a clean douche bottle or irrigation bag to gently flush your vagina
- Limit this to twice weekly for just 2 weeks
4. External Baking Soda Paste for Vulvar Comfort
Sometimes your vulva feels raw or itchy from all that ongoing acidity, and this gentle external treatment can provide sweet relief.
Your comfort recipe:
- Mix equal parts baking soda and water to create a soft, spreadable paste
- Apply externally to affected areas for 5–10 minutes, then rinse thoroughly with warm water
- Use as needed whenever you need some extra comfort
Critical reminder: This paste is for external use only. Never use it inside your vagina.
5. Lifestyle and Supportive Measures
Your daily habits can be powerful allies in both healing and preventing future episodes. If you have a history of VC, consider:
- Switching to pads during your period instead of tampons. Menstrual blood is naturally alkaline and can help reduce lactobacilli levels back to normal ranges.
- Wearing breathable cotton underwear and avoiding tight clothing that creates a hot, moist environment where lactobacilli love to multiply.
- Pausing sexual activity until your symptoms resolve to prevent additional irritation during this healing time.
- Keeping cleansing simple with just warm water and mild, unscented soap. Skip the scented soaps, wipes, or feminine washes that can disrupt your recovering vaginal flora.
6. Press Pause on Probiotics Temporarily
If your supplement contains lactobacillus species, especially those specifically linked to vaginal flora (like lactobacillus crispatus), it's wise to take a break until your cytolytic vaginosis is completely resolved18. These particular strains can increase the number of lactobacilli and worsen that problematic acidity.
Bottom line: When your treatment is specifically tailored to address cytolytic vaginosis, rather than yeast or bacterial vaginosis, you're finally targeting the real culprit instead of just masking symptoms. By gently raising your vaginal pH and giving your vaginal microbiome the time and space it needs to rebalance, you're setting yourself up for lasting comfort and confidence.
Treatments to Avoid
Certain products and treatments can actually make cytolytic vaginosis worse by lowering your vaginal pH even further or feeding that overgrowth of lactobacilli. If you suspect or have been diagnosed with cytolytic vaginosis, these are the things to temporarily avoid:
Lactobacillus-Containing Probiotics (Oral or Vaginal Suppository)
Instead of helping, these can actually fuel the overgrowth of lactobacilli that's causing your discomfort in the first place.
Boric Acid Suppositories
These lower vaginal pH, which is literally the opposite of what cytolytic vaginosis treatment requires.
Vitamin C Tablets or Gels
These acidify your vaginal environment and can make symptoms more intense.
"pH balancing" Washes or Gels
Often marketed as vaginal health heroes, these can actually disrupt the delicate balance you need for recovery.
Regular Douche Use
This can alter your vaginal flora and potentially prolong symptoms.
Here's the thing: these measures can be genuinely helpful for other vaginal conditions like bacterial vaginosis. But in cytolytic vaginosis, they can intensify your discomfort and delay the healing you're working toward. It's all about using the right tool for the right job!
Recovery Outlook with CV
Here's some fantastic news: the prognosis for cytolytic vaginosis is excellent once it's properly identified and managed.
Most people achieve complete symptom resolution with simple, gentle, at-home measures. However, recurrence can happen during hormonal shifts (hello, menstrual cycle changes!) or if those vaginal microbiome triggers persist in your routine.
While chronic, untreated irritation can impact your quality of life, intimacy, and overall vaginal health, serious long-term complications are quite rare19. The key is recognizing what you're dealing with and taking those targeted steps to restore balance.
CV Prevention Strategies
Once you've navigated through cytolytic vaginosis, making a few gentle habit adjustments can help keep your vaginal microbiome in that happy, balanced state and prevent symptoms from making an unwelcome return.
These aren't about micromanaging every aspect of your vaginal health, but creating the optimal environment for your body to do what it does best naturally.
Skip Unnecessary Douche Use
Look, we’ve said this before (actually a few times now), but it’s worth repeating because it’s a HUGE misconception. Regular douching can wash away your protective bacteria and upset that delicate balance of your vaginal flora, sometimes creating the perfect conditions for lactobacilli overgrowth. Stick to gentle, external cleansing with just warm water. Your vagina is naturally self-cleaning and does an amazing job on its own!
Be Mindful With High-Dose Probiotics Unless Your Provider Recommends Them
Probiotics containing lactobacillus species can be wonderful for certain conditions (like BV), but in cytolytic vaginosis, they can tip the scales too far in the wrong direction20.
If you've experienced cytolytic vaginosis before, definitely get medical guidance before adding these supplements back into your routine.
Choose Breathable Fabrics and Change out of Wet Clothes Quickly
Cotton underwear and loose-fitting bottoms help minimize trapped heat and moisture, which can create that lactobacilli-friendly microclimate you want to avoid. After swimming, intense workouts, or particularly hot days, change into dry clothes as soon as you reasonably can.
Consider Pads Instead of Tampons During Menstruation
Your menstrual blood is naturally alkaline and can help raise your vaginal pH back into that ideal balance range. Tampons can trap acidity, making it trickier for cytolytic vaginosis to resolve or stay away for good.
Get Tested Before Treating any Suspected Vaginal Infections
Self-treating without a proper diagnosis can mask the real issue and prolong your discomfort unnecessarily. If you're experiencing ongoing symptoms, ask your healthcare provider to check your vaginal pH and take a look under the microscope before reaching for any antifungal or other treatment.
Track Your Hormone-Related Patterns
If you notice symptoms tend to appear during the luteal phase of your menstrual cycle, make a note of it! Tracking these patterns can help you and your provider take preventive steps before things escalate into full-blown discomfort.
When to See Your Healthcare Provider
Reach out to your healthcare team promptly if you're experiencing:
- Vaginal discharge, itching, or burning that persists for more than a week
- You've tried antifungal treatments without any improvement
- You're dealing with dyspareunia, dysuria, or worsening discomfort
- Symptoms keep recurring in a predictable pattern with your menstrual cycle
- You're genuinely unsure whether you're dealing with candida, bacterial vaginosis, or cytolytic vaginosis
A knowledgeable gynecology or obstetrics provider can perform the right tests and help you avoid the frustration of repeated misdiagnosis. You deserve answers and effective treatment!
Frequently Asked Questions (FAQs)
Can Cytolytic Vaginosis Cause Infertility?
There's no evidence linking cytolytic vaginosis to infertility, but the ongoing discomfort, inflammation, and recurring symptoms can definitely impact your quality of life and sexual well-being if left untreated.
Is Cytolytic Vaginosis Contagious?
Nope! Unlike sexually transmitted infections (STIs), cytolytic vaginosis cannot be passed between partners. However, you might notice symptoms flare after sexual activity due to irritation, so it's worth taking a break from physical intimacy until you're feeling better.
Why Doesn't Antifungal Medication Work for This?
Cytolytic vaginosis is caused by bacteria (specifically an overgrowth of lactobacilli) not Candida, which is a fungus. Antifungal drugs are designed to target fungi, so they simply can't correct the bacterial imbalance that's causing your symptoms.
Can Cytolytic Vaginosis and a Yeast Infection Happen at the Same Time?
It's rare but possible. Since symptoms can overlap so significantly, proper testing is really your best friend for confirming whether one or both conditions are present before starting any treatment.
Will Cytolytic Vaginosis Go Away Without Treatment?
Some cases do resolve naturally over time as your body works to restore balance, but targeted measures like those soothing baking soda sitz baths or suppositories often speed up recovery and reduce your risk of recurrence.
Can I Take Probiotics If I've Had Cytolytic Vaginosis?
Occasional use, such as after a course of antibiotics, may be perfectly fine, but daily lactobacillus species probiotics can raise your lactobacilli levels and lower your vaginal pH, potentially triggering another episode. Your healthcare provider can give you personalized guidance based on your specific situation.
Final Thoughts
Cytolytic vaginosis serves as a gentle reminder that even when it comes to beneficial bacteria, this can be too much of a good thing. The silver lining? With better awareness among both patients and healthcare providers, fewer people will have to endure unnecessary treatments or prolonged discomfort.
The combination of correct diagnosis, targeted care, and smart preventive habits can restore your comfort and help maintain long-term vaginal health. You've got this, and your body's natural wisdom is on your side!
Keep the Conversation Going
- Visit our blog for more women's health tips.
- Join our private Happy V Facebook group to hear from others who've been there.
- Explore supplements designed to support your vaginal health journey.
Disclaimer: This blog is for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Statements about supplements have not been evaluated by the Food and Drug Administration. For more information about vaginal infections, visit the CDC or speak to a licensed healthcare provider.