- Fact Checked
- December 10, 2025
- 5 min read
What Does a Yeast Infection Smell Like?
Table of Contents
Table of Contents
If you’ve ever paused mid-undressing and wondered, “Wait, is that smell… me?!”, you’re definitely not alone. To a large degree, vaginal odor is normal. But when it shifts suddenly or becomes noticeably stronger, it’s worth some investigating, especially if you’re experiencing other symptoms of a yeast infection, like itching and unusual discharge.
So, how do you know what’s normal, what’s not, and when it’s time to call your healthcare provider? Let’s break down what yeast infections smell like (and what they don’t), the role your vaginal microbiome plays, and how to get things back in balance, with science-backed support and zero shame.
This post is for informational purposes only and does not constitute medical advice. See full disclaimer below.
What Does a Yeast Infection Actually Smell Like?
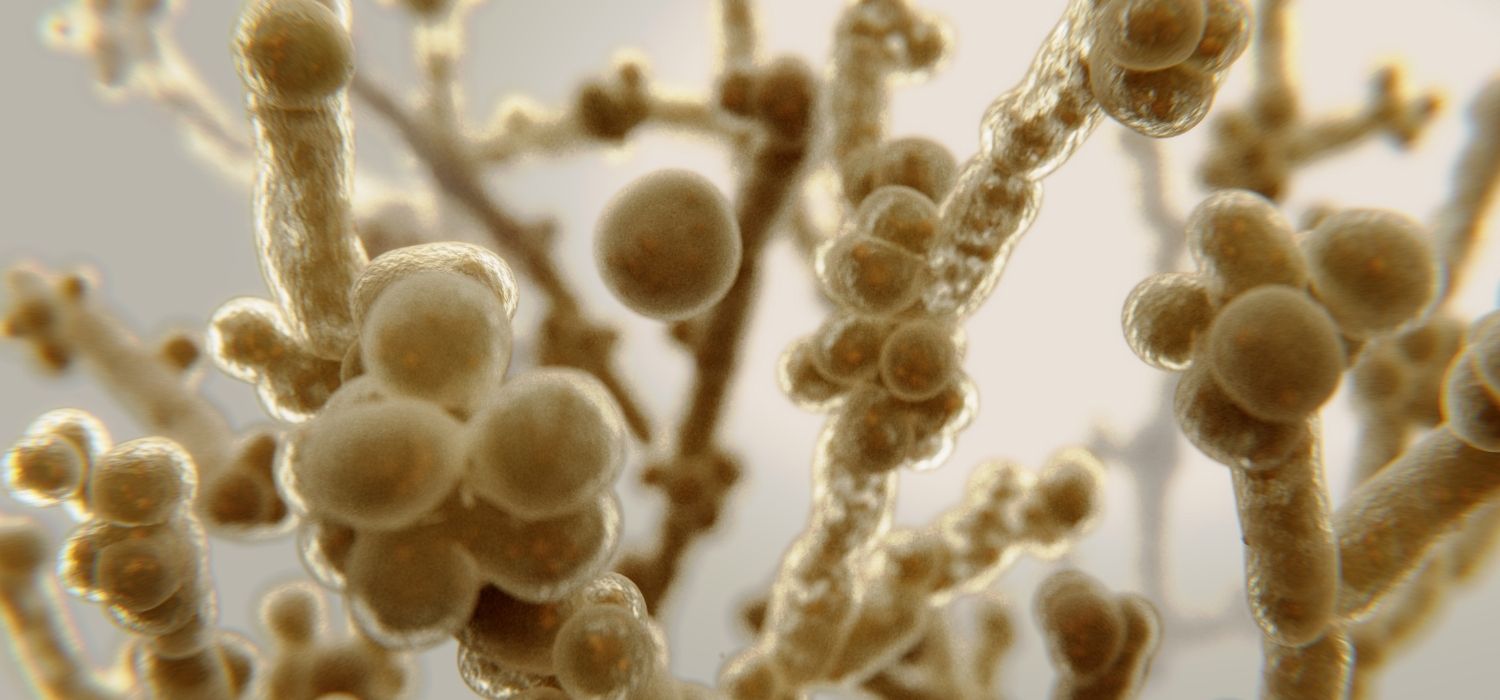
A vaginal yeast infection (also known as vaginal candidiasis) is caused by an overgrowth of the fungus Candida, usually Candida albicans1. While Candida is often present in balanced vaginas, things like antibiotics2, hormonal changes, and even stress can throw off the balance of bacteria in your vaginal microbiome, leading to an overgrowth of yeast.
Though yeast infections often have some pretty noticeable symptoms, a strong or foul-smelling odor usually isn’t one of them3. If there’s any smell at all, it’s often subtle, slightly “yeasty” (think: bread or beer), and not considered unpleasant.
What stands out more are the other symptoms of a yeast infection, such as:
- Thick white vaginal discharge (often described as looking like cottage cheese)4
- Vaginal itching or irritation5
- Redness around the vulva6
- Burning during urination or sex7
Yeast infections are super common8. In fact, the CDC estimates that about 75% of women will get at least one in their lifetime9. Some common causes and risk factors for yeast infections include:
- Antibiotics10
- Hormonal changes from birth control, menopause, or menstruation11
- Tight or synthetic clothing12
- Douching (just… don’t)13
- High sugar intake
- Weakened immune system
- Stress and lack of sleep
When It Might Be Something Else
Even healthy vaginas are not entirely odorless17. But if you are noticing fishy smell or foul-smelling vaginal discharge, it’s typically the sign that something is amiss down there, and that “something” is typically not a yeast infection.
The most common culprits of strong vaginal odors include:
- Bacterial vaginosis (BV): The most common vaginal infection, often accompanied by fishy odor, thin gray discharge, and vaginal irritation
- Trichomoniasis (trich): A sexually transmitted infection (STI) with symptoms that include frothy, yellow-green discharge and a strong, sometimes musty scent18
- Forgotten tampons: A very strong, foul odor often accompanied by dark discharge
If you ever suspect you are experiencing signs of an STI or vaginal infection, call your healthcare provider or gynecologist right away. They will help you pinpoint the exact cause of your odor and help you treat it, so you can avoid future complications.
How to Support Vaginal Health
The first thing you can do to support your vaginal is to see your doctor at the first sign of a vaginal infection and take any medications your doctor recommends exactly as prescribed.
Outside of medications, though, there’s a lot you can do to support and maintain your vaginal health and prevent strong odors from coming back.
- Stop douching: Not only is it unnecessary because the vaginal is self-cleaning, but it can upset your vaginal pH and the balance of Lactobacillus bacteria that protect against infections.
- Wear cotton underwear and avoid tight, non-breathable fabrics in your genital area. Bad bacteria love dark, moist places. Loose bottoms and breathable underwear will keep the vaginal area dry.
- Use condoms. Condoms not only prevent the transfer of STIs and STDs; they also help prevent the spread of bacteria like Gardnerella vaginalis and E. coli, the two biggest causes of BV and UTIs, respectively.
- Avoid scented products, including soaps, sprays, and bubble baths. These often contain harsh chemicals that can disrupt your vaginal flora.
- Adjust your diet. Diets high in added sugars, saturated fats, and processed foods can weaken your immune system and fuel the growth of infection-causing bacteria. Focus on consuming lots of whole foods.
Can Probiotics Help?
Absolutely. Probiotics— and especially those with Lactobacillus strains—play a key role in supporting vaginal health by helping maintain a healthy vaginal pH and crowding out harmful, infection-causing microorganisms. Research shows that replenishing good bacteria can be especially helpful after antibiotics, during hormonal changes, or when dealing with recurring yeast infections or bacterial vaginosis.
That’s where Happy V comes in. Our Prebiotic + Probiotic formula features clinically studied strains like Lactobacillus acidophilus LA-14 and Lactobacillus rhamnosus HN001, which have been shown to support vaginal flora and improve symptoms like itching and discharge.
In preclinical studies, our unique blend demonstrated the ability to inhibit the growth of most Candida species tested, including Candida albicans, the primary cause of vaginal yeast infections. It’s microbiome support that works smarter, so you can feel more balanced, more often.
Final Thoughts
If you’ve noticed changes in odor, discharge, or itching, trust your instincts and don’t hesitate to check in with a healthcare provider. Whether it’s a yeast infection, bacterial vaginosis, or something else, getting clarity is the first step to feeling better.
And if you’re looking to support your vaginal health long-term, consider adding targeted probiotics, dialing in hygiene habits, and tuning in to what your body needs throughout your cycle. When your microbiome is in balance, everything just feels… easier.
Keep the Conversation Going
- Visit our blog for more women's health tips.
- Join our private Happy V Facebook group to hear from others who've been there.
- Explore supplements designed to support your vaginal health journey.
Disclaimer: This blog is for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Statements about supplements have not been evaluated by the Food and Drug Administration. For more information about vaginal infections, visit the CDC or speak to a licensed healthcare provider.
















