- Fact Checked
- November 11, 2025
- 21 min read
Mycoplasma genitalium: The Silent STI You Should Know About
Table of Contents
Table of Contents
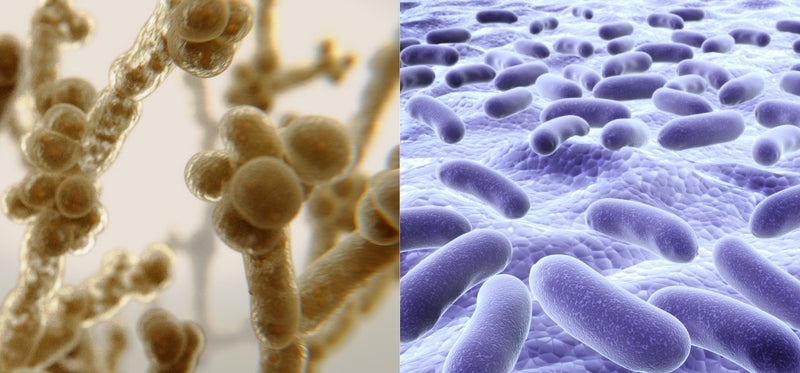
When we talk about sexual health, certain infections tend to hog the spotlight. Think: chlamydia trachomatis, gonorrhea, and syphilis. But there's another bacterial pathogen that's been quietly spreading through communities without getting nearly enough attention. It’s called Mycoplasma genitalium. This little microbe is particularly tricky because it lacks a cell wall, which makes it naturally resistant to certain antibiotics and significantly harder to kick out of your body once it moves in.
The Centers for Disease Control and Prevention (CDC) has identified Mgen as a leading cause of nongonococcal urethritis (NGU) and cervicitis1. Yet healthcare providers estimate its prevalence is seriously underestimated because so many cases fly under the radar with zero symptoms. That's exactly why awareness is so crucial. You might have Mgen, feel completely normal, and still be at risk for serious complications down the road.
This post is for informational purposes only and does not constitute medical advice. See full disclaimer below.
What Is Mycoplasma genitalium?

Mycoplasma genitalium is a sexually transmitted bacterial infection that primarily affects the urogenital tract (aka the urethra, bladder, ureters, and kidneys) in both men and women2.
Scientists first identified M. genitalium infection back in the early 1980s3. It’s one of the smallest known bacteria that can cause disease in humans, and recent epidemiology data and meta-analysis studies are showing it's way more common than anyone previously thought, especially among people with multiple sexual partners or a history of other sexually transmitted diseases.
The fact that it lacks a cell wall is absolutely crucial to understand. This means that antibiotics targeting cell wall synthesis, like penicillins and cephalosporins that are commonly used for UTIs and other infections, are completely ineffective against Mgen4. You could take amoxicillin or cephalexin all day long, and it wouldn't touch this infection.
Making matters worse, we're seeing rising rates of macrolide resistance and fluoroquinolone resistance, which makes treatment increasingly complicated and sometimes requires multiple rounds of different antibiotics.
Transmission and Risk Factors
As an STI, Mgen spreads through sexual contact. Most people assume this just means vaginal sex, but it includes anal sex and possibly oral sex, too5.
The really frustrating part is that it can be passed along even when someone has absolutely no symptoms, which means you could unknowingly give it to or receive it from a partner.
Your risk of contracting Mgen goes up if you have:
- Multiple or new sex partners
- Inconsistent condom use
- A history of other STIs
- Are younger (where incidence rates tend to be higher)
But honestly, anyone who's sexually active could potentially encounter this infection (and suffer the potential consequences from lack of treatment).
Symptoms of Mycoplasma genitalium

Here's where Mycoplasma genitalium gets really sneaky. Some people never notice anything is wrong at all. In fact, research shows that seven to eight out of every ten men and five to seven out of every ten women with Mgen have absolutely no symptoms. And when symptoms do appear, they can be surprisingly variable and easily overlooked.
Timeline and Onset
When symptoms do develop, they typically show up 1-3 weeks after initial infection, though the timeline can vary significantly from person to person.
Some people might notice symptoms right away, while others might not experience anything for weeks or even months.
Even more confusing, symptoms can:
- Appear and then disappear on their own temporarily
- Fluctuate in intensity over time
- Be so mild they're attributed to other causes like stress or minor irritation
- Worsen during times when your immune system is compromised
Symptom Severity and Presentation
The range of symptoms can go from barely noticeable to quite uncomfortable, and understanding this spectrum is important for recognizing potential infections.
They also differ between men and women.
For women, symptoms might include:
- Mild to moderate cervicitis
- Abnormal vaginal discharge (which can range from slightly different than usual to obviously problematic)
- Pelvic pain that might come and go
- Bleeding after sex (from light spotting to more noticeable bleeding)
- Burning sensation during urination (anywhere from mild discomfort to significant pain)
For men, Mycoplasma genitalium symptoms typically present as:
- Urethritis or nongonococcal urethritis6
- Discharge from the urethra (ranging from barely visible to obvious)7
- Painful urination (from slight discomfort to sharp burning)
- Occasional testicular discomfort
Extragenital Symptoms
Mgen can also affect other areas of the body and even create symptoms in other areas of the body, though, as you can read, these symptoms do not initially scream “STI,” but can easily be attributed to gut issues or even the common cold:
- Rectal infections are usually silent, but when symptoms occur, they might include rectal discomfort, discharge, or pain during bowel movements8
- Pharyngeal infections rarely cause symptoms, though some people might experience mild throat discomfort9
When Symptoms Overlap with Other Conditions
As if all these vague symptoms aren’t confusing enough, Mgen symptoms can also present like several non-STI conditions:
-
Urinary tract infections can cause the same burning during urination
-
Yeast infections might produce similar discharge patterns in women
- Prostatitis in men can cause similar urethral discomfort
-
Bacterial vaginosis can create similar vaginal symptoms
The key difference is that these other conditions usually respond to their typical treatments, while Mgen symptoms will persist despite standard UTI or yeast infection treatments.
Factors That Influence Symptoms
Whether or not you experience Mgen symptoms and how intense those symptoms are is often influenced by things like:
- Your menstrual cycle: Some women notice symptoms worsen at certain times of the month
-
Co-infections: Having other STIs at the same time can intensify symptoms or change how they present
- Overall immune health: Stress, illness, or immunocompromising conditions might affect symptom severity
Menstrual Cycle Tracking
How Do You Track Your Menstrual Cycle And Why Does It Matter for Your Health?
How Mycoplasma genitalium Compares to Other Infections

Understanding how Mgen stacks up against other common infections can help you make sense of what you might be experiencing and why specific testing matters so much.
Mgen vs. Chlamydia
Both can cause cervicitis and urethritis with very similar symptoms10, making them nearly impossible to distinguish without testing. However, there are some key differences:
- Treatment complexity: Chlamydia typically responds well to standard first-line antibiotics, while Mgen often requires specialized treatment due to antimicrobial resistance
- Testing: Chlamydia shows up on routine STI screening panels, while Mgen requires a specific NAAT test11
-
Resistance patterns: Mgen has developed significant resistance to macrolide antibiotics, making treatment more challenging
Mgen vs. Gonorrhea
These infections can cause similar urethritis and cervicitis, but there are notable differences:
- Symptom intensity: Gonorrhea often produces more obvious, uncomfortable symptoms that prompt people to seek medical attention faster
- Detection: Gonorrhea appears on standard STI screening panels that most healthcare providers routinely order12
-
Treatment response: While gonorrhea has developed some antibiotic resistance, treatment protocols are more established and generally effective
Mgen vs. Bacterial Vaginosis (BV)
It's important to understand that BV isn't actually an STI; it's an imbalance of your vaginal microbiome13. However, both conditions share some similarities:
-
Discharge patterns: Both can cause abnormal vaginal discharge
- PID risk: Both increase your risk of developing pelvic inflammatory disease
- Microbiome impact: Both can disrupt healthy vaginal flora, which is why probiotic support becomes crucial, especially after antibiotic treatment
Mgen vs. Trichomoniasis
These represent two completely different types of organisms. Trich is caused by a parasite14, while Mgen is bacterial. Here are some other ways they compare:
- Symptom visibility: Trich sometimes causes more obvious symptoms like frothy discharge or strong odor15
-
Transmission: Both can be completely asymptomatic while still being highly transmissible
- Treatment approach: They require entirely different types of medications
Overview: Mgen vs. Other Common Infections
Here is a chart that compares Mgen with other common infections when it comes to type of pathogen, transmission, symptoms, treatment, and prevention.
While information is empowering, remember the goal of this chart is not to help you diagnose yourself. That’s something that’s always best left to a gynecologist or other healthcare provider.
| Feature |
Mycoplasma genitalium (Mgen) |
Chlamydia | Gonorrhea |
Bacterial Vaginosis (BV) |
Trichomoniasis (Trich) |
| Type of Pathogen | Bacterium without a cell wall | Bacterium (Chlamydia trachomatis) | Bacterium (Neisseria gonorrhoeae) | Microbiome imbalance (not an STI) | Parasite (Trichomonas vaginalis) |
| Transmission | Vaginal, anal sex, possible oral sex | Vaginal, anal, oral sex | Vaginal, anal, oral sex | Not sexually transmitted | Vaginal, anal, oral sex |
|
Common Symptoms |
Urethritis, cervicitis, abnormal vaginal discharge, pelvic pain | Similar to Mgen – cervicitis, urethritis | More severe discharge, burning, pelvic pain | Thin/gray discharge, odor | Frothy/yellow-green discharge, odor, irritation |
|
Asymptomatic Rates |
Very high (up to 70% in men, 50% in women) | High (~70%) | Lower than Mgen | Moderate | ~70% can be asymptomatic |
| Screening Availability | Not on routine STI panels; requires NAAT | Included in most STI panels | Included in most STI panels | Diagnosed via pelvic exam/lab | Diagnosed via pelvic exam/lab |
| Antibiotic Resistance | Macrolide resistance and fluoroquinolone resistance increasing16 | Rare | Significant but better-studied | Not applicable | Not significant |
| First-Line Treatment | Doxycycline then targeted antibiotic (azithromycin or moxifloxacin)17 | Azithromycin or doxycycline18 | Ceftriaxone injection + doxycycline/azithromycin19 | Antibiotics (metronidazole, clindamycin)20 | Metronidazole or tinidazole21 |
| Complications if Untreated | PID, infertility, ectopic pregnancy, increased risk of HIV infection | PID, infertility, ectopic pregnancy | PID, infertility, systemic infection | Increased risk of STIs, pregnancy complications | PID, infertility, adverse pregnancy outcomes |
| Prevention | Condoms, partner treatment, regular Mycoplasma genitalium testing, microbiome support | Condoms, testing | Condoms, testing | Vaginal health support, avoid irritants | Condoms, testing |
Diagnosis and What to Expect from Testing

Getting an accurate Mgen diagnosis requires a nucleic acid amplification test (NAAT), which is essentially a molecular assay that hunts for Mgen's genetic material in your system.
Your healthcare provider will collect either a swab from your cervix, vagina, or urethra, or ask for a urine sample. The process itself is quick and straightforward, similar to getting tested for chlamydia or gonorrhea.
Here's what makes Mgen testing different: given the growing rates of macrolide resistance we're seeing, many clinicians now also recommend resistance testing before prescribing any antibiotics. This extra step helps prevent treatment failure and saves you from unnecessary exposure to drugs that won't actually work against your specific strain of the infection.
After providing your vaginal swab or urine sample, you should expect results within a few days to a week, depending on your healthcare provider's lab setup.
If you test positive, don't panic. While Mgen is trickier to treat than some other STIs, it is absolutely treatable with the right approach, and resistance testing will help determine what that “right approach” is.
Treatment Options for Mycoplasma genitalium

Treating Mycoplasma genitalium effectively means using the right antibiotic at the right time, ideally guided by (you guessed it) resistance testing.
Because Mgen has no cell wall and is showing rising macrolide resistance (and even some fluoroquinolone resistance), following a structured approach increases your odds of success and helps prevent treatment failure.
First-Line Treatment
Most people will start with doxycycline 100 mg taken orally twice daily for 7 days. This isn’t because doxycycline alone cures Mgen (it usually doesn’t!), but because it reduces bacterial load, making the follow-up antibiotic more effective.
If Resistance Testing Is Available
When your healthcare provider can run a resistance test before prescribing, follow-up treatment is tailored to your strain’s susceptibility:
-
If the infection is macrolide-sensitive: You’ll follow doxycycline with azithromycin — 1 g orally as a starting dose, then 500 mg once daily for 3 more days (a total of 2.5 g).
- If the infection is macrolide-resistant: You’ll follow doxycycline with moxifloxacin 400 mg orally once daily for 7 days.
This “resistance-guided” approach offers higher cure rates and reduces the risk of creating even more resistant strains.
If Resistance Testing Is Not Available
In areas or clinics where resistance testing isn’t an option, most providers now assume high macrolide resistance and go straight from doxycycline to moxifloxacin. This avoids wasting time and risking failure with azithromycin in resistant cases.
Alternative or Second-Line Treatments
If symptoms persist even after first-line care and follow-up antibiotics, an infectious diseases specialist may recommend other regimens, such as:
-
Doxycycline for 7 days followed by pristinamycin 1 g four times daily for 10 days.
- Minocycline 100 mg twice daily for 14 days.
These are reserved for special circumstances, since clinical data on their success is limited and some carry a higher risk of side effects.
Partner Treatment Is Non-Negotiable
No matter which regimen is used, all sex partners from the past 60 days should be notified, evaluated, and treated, even if they have no symptoms and even if their test results aren’t back yet. Without partner treatment, there’s a high risk of passing the infection back and forth (“ping-pong” reinfection).
Both you and your partners should avoid sexual activity at least until treatment is complete, not just until any symptoms subside. Ideally, though, you would wait until treatment is complete and a test of cure confirms the infection is gone.
Special Considerations
Though treatment for Mgen is highly individualized as it is, special considerations need to be made when treating pregnant women or those with HIV.
-
Pregnancy: Some first-line antibiotics, like doxycycline, are not safe during pregnancy. If there’s any chance you may be pregnant, tell your healthcare provider so they can select an alternative, pregnancy-safe regimen.
-
People with HIV: Current treatment guidelines recommend the same antibiotic regimens for people living with HIV as for those without, but closer follow-up may be advised to ensure complete clearance.
-
People with other health conditions: If you have liver problems, kidney issues, or are taking other medications, make sure your healthcare provider knows this before starting treatment, as it might affect which antibiotics are safest and most effective for you.
Why Completing Your Full Antibiotic Course is Crucial
This might seem obvious, but it's worth emphasizing: taking every single dose of your prescribed antibiotics exactly as directed isn't just important for your personal health; it's critical for public health, too.
When infections are only partially treated, the bacteria that survive are often the ones that were already slightly better at resisting the antibiotic. These survivors then multiply and pass on their resistance mechanisms, creating stronger, harder-to-treat strains. This is a particular concern with Mgen, which is already resistant to so many antibiotics due to its lack of cell wall.
If your healthcare provider prescribes you antibiotics for Mgen, here are some practical tips to stay on top of it and avoid antibiotic resistance:
- Set phone alarms for each dose
- Use a pill organizer to track what you've taken
- Ask your partner or a trusted friend to help remind you
- Keep your medication somewhere you'll see it regularly
Test of Cure: Confirming Treatment Success
A test of cure is exactly what it sounds like, a follow-up test to confirm that your treatment actually worked and the infection is completely gone.
Who needs a test of cure?
- People who had persistent symptoms during or after treatment
- Anyone treated with alternative regimens due to treatment failure
- People with complications like PID who want confirmation of cure
- Those at high risk for complications (like people trying to conceive)
Who doesn't need a test of cure?
- Asymptomatic people who received a recommended first-line regimen and completed it fully
- People whose symptoms completely resolved during treatment and who received standard recommended therapy
When to test
Wait at least 3-4 weeks after completing your antibiotic course before doing the test of cure. Testing too early might give false results since bacterial fragments can still be detected even after successful treatment.
Why it matters
Confirming eradication prevents unknowing transmission to partners and helps identify cases that need additional treatment, but unnecessary testing can lead to false positives and overtreatment.
What to Do if Treatment Doesn't Work
Sometimes, despite following all the right steps, symptoms don't improve or they come back after treatment. This can be incredibly frustrating and anxiety-provoking, but there are clear next steps you can take.
If your symptoms don't resolve or return after completing treatment, contact your healthcare provider right away. Persistent symptoms might indicate:
-
Undetected antibiotic resistance that wasn't caught in initial testing
-
Reinfection from an untreated partner
-
Treatment failure requiring a different antibiotic approach
-
Co-infection with another organism causing similar symptoms
Your provider might recommend repeating resistance testing, trying a different antibiotic regimen, or referring you to a specialist who has more experience managing complicated Mgen cases.
Follow-Up Care and Monitoring After Treatment
Understanding what to expect after completing treatment can help reduce anxiety and ensure you're monitoring your health appropriately.
Most people who complete a recommended regimen and have no symptoms don't need routine follow-up visits. If you had symptoms before treatment, pay attention to whether they fully resolve within a few weeks of completing antibiotics. Keep track of any new or returning symptoms, especially if they appear weeks or months after treatment
Contact your healthcare provider if you ever have:
- Symptoms that persist more than 2-3 weeks after completing treatment
- New symptoms that develop after treatment was completed
- Any symptoms that return after initially resolving
- Concerns about side effects from medications
The Importance of Treatment Failure Reporting
When standard treatments don't work, it's not just frustrating for you; it's valuable information for the broader medical community. Healthcare providers and health departments can report Mgen treatment failures through specialized registries that help track resistance trends and inform future treatment guidelines.
If you experience treatment failure, encourage your healthcare provider to report it. This data helps researchers understand how resistance patterns are changing and contributes to developing better treatment protocols for everyone. It's one way your experience can help improve care for others dealing with similar challenges.
Managing the Emotional and Practical Challenges of Treatment
Dealing with a resistant infection can be emotionally exhausting and stressful. It's completely normal to feel frustrated, anxious, or overwhelmed when standard treatments don't work as expected. Here's how to navigate these challenges:
Communicating with your healthcare provider:
Don't hesitate to ask questions about your treatment plan. Be honest about any side effects you're experiencing. Request clear timelines for when you should expect improvement, and ask about what to do if symptoms don't resolve
Taking care of yourself emotionally:
Remember that treatment failure doesn't mean you did anything wrong. Connect with trusted friends or family for support, and consider speaking with a counselor if the stress becomes overwhelming
Self-advocacy tips:
Keep a symptom diary to track your progress. Research your treatment options so you can have informed discussions with your provider, and don't be afraid to seek a second opinion if you feel your concerns aren't being addressed
Long-Term Prognosis After Treatment
The good news about long-term prognosis after successful Mgen treatment is that most people go on to have perfectly normal reproductive and sexual health.
However, the infection can cause some lasting damage if it was present for a long time before treatment, particularly if it progressed to PID. That's why early detection and prompt treatment are so crucial.
Partner Disclosure & Treatment

If you test positive for M. genitalium infection, having a conversation with your sex partners isn't optional; it's absolutely critical, even if they have no symptoms and even if it feels super awkward.
Because this infection loves to stay silent, partners might unknowingly pass it back to you or spread it to others without having any idea what's happening.
When you talk to partners, share your diagnosis clearly and explain that Mycoplasma genitalium testing requires a specific test. It doesn’t show up on standard STI panels.
Encourage them to see a healthcare provider for proper evaluation, resistance testing, and appropriate treatment.
Sexual Activity During Treatment
This is crucial: you must abstain from all sexual activity until both you and all your partners have completed the full course of treatment. If a test of cure is recommended for anyone involved, wait until those results confirm the infection is completely gone before resuming sexual activity.
For people with pelvic inflammatory disease, the guidelines are even more specific: refrain from intercourse until 14 days after the start of treatment or 14 days after symptoms have completely resolved, whichever comes later.
Key timing guidelines:
- No sexual activity during the entire treatment period for all partners
- If test of cure is needed, wait until negative results are confirmed
- For PID cases, wait at least 14 days after treatment starts or symptoms resolve
- Even if you feel better quickly, complete the full waiting period to prevent reinfection
What Happens if Mycoplasma genitalium Goes Untreated?

When M. genitalium infection goes untreated, it doesn’t just linger; it can slowly move from the lower to the upper urogenital tract, where the damage can become more serious and sometimes permanent.
In women, untreated Mgen may:
- Cause pelvic inflammatory disease (PID), leading to inflammation and scarring of the fallopian tubes22.
- Increase the risk of ectopic pregnancy (when a fertilized egg implants outside the uterus)23.
- Contribute to infertility if the reproductive tract is damaged over time.
In men, the infection can cause:
- Persistent urethritis or nongonococcal urethritis (NGU), which may last for months.
- Ongoing pain, burning, or discharge from the urethra, even in the absence of other symptoms.
There’s also a broader public health impact. Untreated Mgen can put you at increased risk of acquiring or transmitting other sexually transmitted infections, including HIV infection and chlamydia. The longer it remains in the body, the greater the likelihood of complications, making timely Mycoplasma genitalium testing, proper treatment, and thorough partner management essential for protecting both individual and community sexual health.
Prevention Strategies

Protecting yourself from Mgen and other sexually transmitted infections isn't about just doing one right thing; it's about creating multiple layers of protection that work together.
Barrier Protection and Safe Sex Practices
Consistent barrier protection is your first line of defense. Condoms and dental dams help prevent Mgen transmission during vaginal, oral, and anal sex. While they're not 100% foolproof, they significantly reduce your risk.
Limiting your number of sexual partners naturally lowers your odds of exposure to Mgen and other STDs, but this doesn't mean you have to live like a monk. It's about being intentional and informed about your choices.
Regular Testing and Health Monitoring
Regular testing is crucial, especially if you have risk factors or multiple partners. Even without symptoms, periodic Mycoplasma genitalium testing can catch infections early when they're easier to treat and before they cause complications.
Key testing recommendations:
- Request specific Mgen testing if you have symptoms that don't resolve with standard UTI or yeast infection treatment
- Include Mgen testing in your regular STI screening if you have multiple partners
- Get tested if a partner is diagnosed with Mgen, even if you feel fine
Supporting Your Vaginal Microbiome
Antibiotics, while necessary for clearing M. genitalium infection, don’t discriminate. They target harmful bacteria and the population of beneficial Lactobacillus species that help keep your vaginal environment balanced and resilient24.
When the vaginal microbiome loses these protective bacteria, the door can open to recurring infections, changes in pH, and even the overgrowth of other sexually transmitted infections or opportunistic pathogens.
That’s where Happy V’s Prebiotic + Probiotic comes in. Doctor-formulated with clinically studied strains such as Lactobacillus rhamnosus and Lactobacillus reuteri, they’re designed to:
- Replenish protective bacteria that help maintain optimal vaginal pH.
- Support post-antibiotic recovery, reducing the likelihood of microbiome imbalance.
- Promote an inhospitable environment for pathogens, helping to lower recurrence risk after treatment.
Incorporating Happy V Probiotics into your post-treatment care is like giving your vaginal health a recovery partner, one that works to restore your body’s natural defenses so you can feel confident, balanced, and ready to move forward.
Communication and Partner Health
Open communication about sexual health creates the foundation for everything else. Having honest conversations with partners about STI testing history, protection preferences, and sexual health priorities makes prevention so much more effective.
Final Thoughts
Mycoplasma genitalium might not make headlines like other STIs, but it absolutely deserves a spot on your sexual health radar. Its sneaky ability to stay hidden combined with rising antimicrobial resistance rates makes it a genuine public health concern that affects real people in real relationships.
The empowering part is that you have so much control over this situation. By staying informed, getting tested regularly, treating infections promptly, involving partners in your care, and taking proactive steps to prevent reinfection, you're protecting both your reproductive health and your community's wellbeing.
Keep the Conversation Going
- Visit our blog for more women’s health tips.
- Join our private Happy V Facebook group to hear from others who've been there.
- Explore supplements designed to support your vaginal health journey.
Disclaimer: This blog is for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Statements about supplements have not been evaluated by the Food and Drug Administration. For more information about vaginal infections, visit the CDC or speak to a licensed healthcare provider.