- Fact Checked
- November 12, 2025
- 6 min read
BV vs. Yeast Infection: How to Tell the Difference and Get Relief
Table of Contents
Table of Contents
Unusual discharge is definitely a sign of BV, right? Or is it a yeast infection?
If you’ve ever asked yourself that in the bathroom mirror, you’re far from alone. Changes in vaginal discharge, itching, or weird smells can leave you guessing whether it’s bacterial vaginosis, a yeast infection, or something else entirely.
Once you understand what sets these two vaginal infections apart, from causes to symptoms to treatment, you’ll feel way more confident about what’s normal, what’s not, and when to call your healthcare provider for backup.
This post is for informational purposes only and does not constitute medical advice. See full disclaimer below.
What Is Bacterial Vaginosis (BV)?
Bacterial vaginosis is the most common form of vaginitis in women ages 15 to 44. According to the Centers for Disease Control and Prevention (CDC), it affects nearly 21 million women every year—and that’s just in the United States1!
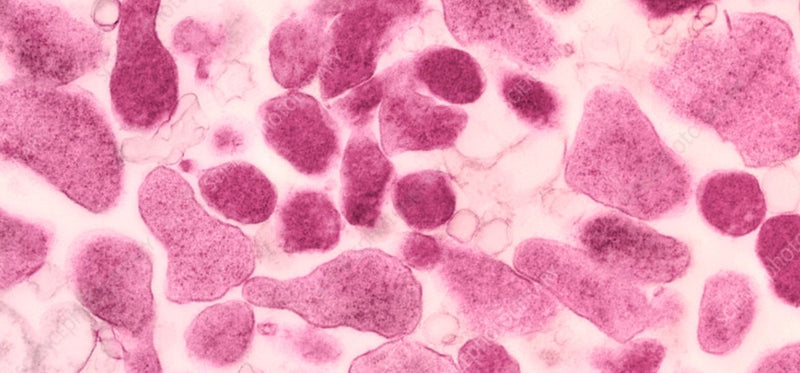
BV happens when the normal balance of good lactobacilli bacteria and bad bacteria gets thrown off, leading to an overgrowth of certain types of bacteria, with the most common being Gardnerella vaginalis2.
Most women who have BV actually experience no symptoms. These asymptomatic cases tend to clear up on their own.
Those who do experience BV symptoms often experience:
- Thin, watery vaginal discharge that’s grayish or white
- A strong fishy odor, especially after sexual activity
- Mild vaginal itching or burning when you pee
Remember that even mild symptoms are your body’s way of telling you it needs support. Reach out to a gynecologist or other healthcare professional at the first sign of discomfort.
What Is a Yeast Infection?
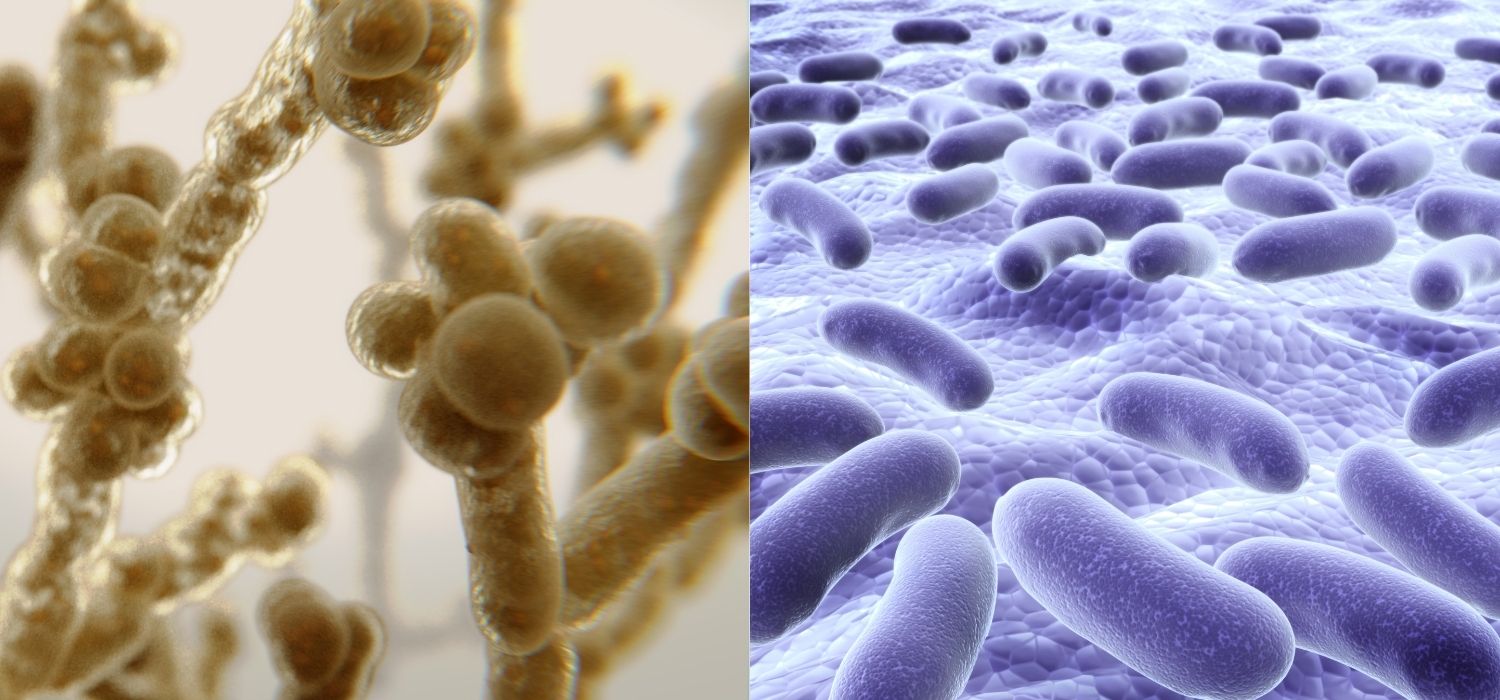
A yeast infection, also known as vaginal candidiasis, is caused by an overgrowth of the Candida fungus (most often Candida albicans) that naturally lives in your vagina3.
Your healthy vaginal flora with good levels of lactobacilli usually keep Candida in check but when something throws off this natural balance (like antibiotics, hormonal changes, or a weakened immune system), the fungus can multiply, leading to symptoms.
Classic symptoms of a yeast infection include:
- Thick, white, clumpy “cottage cheese” discharge
- Intense vaginal itching or redness around the vulva
- A burning sensation when you pee or during sex
You can see how these symptoms overlap with BV, and even with urinary tract infections (UTIs). That’s why it’s so important to get a doctor’s diagnosis before beginning any kind of treatment—you need to make sure you’re treating the right infection!
Causes & Risk Factors
Though one infection is caused by bacteria and another by a fungus, both BV and yeast infections are triggered by a disruption to your vaginal flora, one that affects the levels of infection-fighting lactobacilli.
Common BV triggers include:
- Douching, which disrupts your vaginal pH
- New or multiple sexual partners
- Using scented soaps or body washes, sex toys that aren’t properly cleaned, or sitting in hot tubs often
Common yeast infection triggers include:
- Taking antibiotics or birth control pills
- High blood sugar (especially if you have diabetes)
- Wearing tight, non-breathable clothing instead of cotton underwear
- Hormonal changes from menopause, pregnancy, or estrogen fluctuations
How to Tell the Difference
Sometimes it’s tricky because BV and yeast infections can show up with similar symptoms, like discharge or discomfort. But there are clues:
- Smell: BV usually comes with a fishy odor; yeast infections do not4.
- Discharge texture: BV discharge is thin and watery; yeast infection discharge is thick, lumpy, and looks like cottage cheese5.
- Itch factor: Itching is more common and intense with a yeast infection6.
Here’s something that complicates things a bit: other vaginal infections and even some STIs can mimic symptoms of BV of a yeast infection, too. That’s why the best person to diagnose a vaginal infection is your gynecologist or healthcare provider. They may test your vaginal pH, take a swab, or look under a microscope to confirm if it’s bacterial vaginosis, candidiasis, or something else entirely. From there, they can prescribe the best, most effective treatment.
How to Treat BV vs. Yeast Infections
Whether your doctor ultimately diagnoses you with BV7 or yeast infections, the good news is both are highly treatable through antibiotics or antifungals.
BV Treatment Options
To treat BV, your doctor may prescribe antibiotics like metronidazole, clindamycin, or tinidazole8. These come as either pills or vaginal suppositories. With antibiotics, it’s always important to finish the full dose, even if your symptoms of BV clear up. This prevents recurrence and reduces the chances of antibiotic resistance.
Yeast Infection Treatment Options
Most yeast infections can be treated with over-the-counter (OTC) antifungal medications, like miconazole, clotrimazole, or Monistat suppositories or vaginal creams9. It’s always best to confirm the best option with your healthcare provider before running to the pharmacy. Some people need a single-dose oral medication like fluconazole (Diflucan).
Preventing BV & Yeast Infections At Home
After you’ve finished any prescribed treatments, you need to think about how you’ll prevent these infections from coming back. For many women, this involves simple changes to their daily routine.
To maintain good vaginal health:
- Wear breathable cotton underwear and avoid tight clothes.
- Skip douching and heavily scented soaps and wash your vulva with mild soap and warm water only.
- Wash sex toys thoroughly after every use.
- Use condoms to prevent the spread of harmful bacteria during sex.
- Watch for triggers like antibiotics, birth control pills, or hormonal changes.
Where Probiotics Come In
Your daily habits matter, but so does your internal balance. Happy V’s Prebiotic + Probiotic is designed to help restore and rebalance lactobacilli levels, supporting healthy vaginal pH and fighting the overgrowth of bad bacteria or Candida.
In preclinical studies, Happy V’s unique blend showed promising activity against the overgrowth Candida albicans, the main cause of vaginal yeast infections, and also helped keep Gardnerella vaginalis, a common culprit for BV, in check10.
When your microbiome is strong, your vagina is strong, so you can spend less time worrying about vaginal infections and more time living life.
Final Thoughts
BV and yeast infections are common, treatable, and nothing to feel embarrassed about. Listen to your body, watch for changes in your vaginal discharge, and don’t hesitate to see your OB-GYN if something feels off.
With smart habits, doctor-recommended antifungal medications or antibiotics when needed, and daily probiotic support, you’ve got all the tools you need to stay balanced, comfortable, and empowered.
Keep the Conversation Going
- Visit our blog for more on BV treatment options and women's health tips.
- Join our private Happy V Facebook group to hear from others who've been there.
- Explore supplements designed to support your vaginal health journey.
Disclaimer: This blog is for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Statements about supplements have not been evaluated by the Food and Drug Administration. For more information about vaginal infections, visit the CDC or speak to a licensed healthcare provider.