- Fact Checked
- November 14, 2025
- 6 min read
Can BV Cause Pelvic Inflammatory Disease?
Table of Contents
Table of Contents

For women dealing with recurrent bacterial vaginosis (BV), it can be tempting to brush off symptoms like unusual vaginal discharge or a fishy odor. But here’s the thing: you should never ignore or just “put up with” uncomfortable symptoms.
Beyond taking a toll on your confidence, mental health, and relationships, untreated BV can actually increase your risk of developing pelvic inflammatory disease (PID), a serious condition that affects your upper reproductive organs, including the cervix, uterus, fallopian tubes, and ovaries.
Your vaginal health deserves your attention, and you deserve to feel confident, comfortable, and cared for every step of the way. So let’s talk about the link between BV and PID, how to spot the signs of a worsening BV infection, and how to prevent symptom flare-ups.
This post is for informational purposes only and does not constitute medical advice. See full disclaimer below.
What is Bacterial Vaginosis?

Bacterial vaginosis, or BV, is the most common vaginal infection in women of reproductive age1. It occurs when the normal balance of bacteria in your vagina shifts, causing an overgrowth of harmful bacteria (usually Gardnerella vaginalis).
When there are more bad bacteria in your microbiome than good, you can experience symptoms of bacterial vaginosis like:
- Thin, grayish vaginal discharge2
- A strong fishy odor, especially after sex
- Mild vaginal itching or burning sensation
Factors like multiple sexual partners, douching, using scented soaps and tampons, or hormonal changes, like those that happen during menopause, pregnancy, or while on birth control pills, can all increase your risk of BV3.
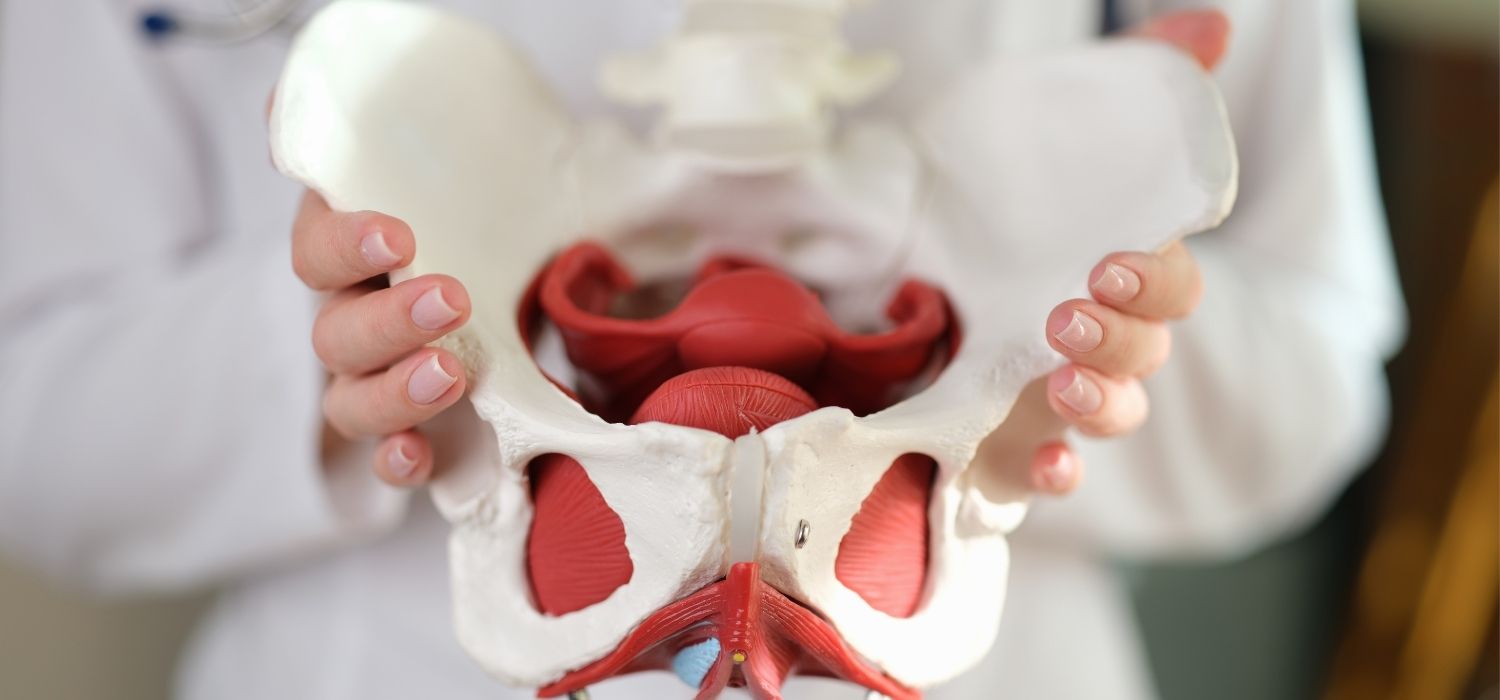
What is Pelvic Inflammatory Disease (PID)?

Pelvic inflammatory disease is an infection of the upper reproductive system4. It develops when bacteria (like those from untreated BV or sexually transmitted infections like chlamydia or gonorrhea) travel up from the vagina and cervix to the uterus, fallopian tubes, and ovaries5.
Over time, untreated PID can lead to:
- Scarring of the reproductive organs6
- Chronic pelvic pain
- Infertility
- Ectopic pregnancy
So while BV doesn’t directly cause PID, it sets the stage for other harmful bacteria to get comfortable and move upward, especially if it’s left untreated.
What’s the Link Between BV and PID?
We mentioned how the bacteria that cause BV can eventually lead to PID if not addressed through antibiotic treatment and other interventions. And while it’s important to know that BV is not a sexually transmitted disease (STD)7, it does increase your risk of getting a sexually transmitted infection (STI). This can also increase your chances of getting PID, since untreated STIs like chlamydia are the most common cause of PID.

How does BV increase your chances of an STI? The bacteria that cause BV weaken your vaginal defenses, making it easier for other pathogens to spread, especially if you’re sexually active with multiple sexual partners or practice douching.
When to Call Your Healthcare Provider
Any sign of a vaginal infection, like unusual discharge or odor, is a sign to see your healthcare provider. This is especially true if you notice your symptoms aren’t improving or are getting worse.

Talk to your healthcare provider if you notice:
- Changes in vaginal discharge that are new or worsening
- New or intense pelvic pain or discomfort in your lower abdomen
- Pain during sexual intercourse
- Unusual vaginal bleeding outside of your period
- Fever or chills
A quick pelvic exam can help rule out PID, cervicitis, or other vaginal infections.
Treatment Options for BV and PID
The good news is that both BV and PID are treatable through antibiotics8, though which antibiotics are used differ based on your diagnosis.

For BV, your doctor may prescribe antibiotics like metronidazole, clindamycin, or suppositories9.
For PID, stronger antibiotics are usually needed and, depending on your symptoms, your doctor may advise a hospital visit, too.
As with all prescribed treatments (and especially antibiotics!) it’s important to complete your course exactly as prescribed, even if your symptoms have gotten better or resolved. This will help you clear the infection completely and prevent recurrence, which can be harder to treat.
How to Prevent BV and PID
As they say, prevention is the best treatment. And luckily, effectively preventing both BV and PID often comes down to some simple changes in lifestyle and daily habits.

Taking small steps every day can help keep your vaginal microbiome balanced:
- Use condoms or dental dams during sexual contact
- Skip douching and scented soaps that disrupt your natural flora
- Wear breathable cotton underwear and change out of swimsuits and sweaty clothes ASAP
- Stay on top of STI screenings, especially if you have a new or multiple sexual partners
Support Your Vaginal Health with Probiotics
In addition to smart habits, daily probiotics may help maintain your natural balance of bacteria, keeping up the levels of healthy bacteria to prevent the overgrowth of bad. Happy V’s doctor-formulated Prebiotic + Probiotic includes clinically studied strains to support healthy levels of lactobacilli (aka your vagina’s best defenders).
In fact, Happy V’s preclinical data show our blend helps keep Gardnerella vaginalis (the main BV troublemaker) from overgrowing. When you combine probiotics with lifestyle habits, you’re giving your vagina daily support to bounce back after antibiotics and reduce your risk of recurrent bacterial vaginosis, vaginitis, or pelvic inflammatory disease.
Final Thoughts
Bacterial vaginosis is super common and nothing to be ashamed of. But it’s never something to ignore, either. Staying informed, getting the right treatment, and supporting your vaginal microbiome can help protect your reproductive organs from serious complications like PID. When in doubt, talk to your healthcare provider and remember, your vagina works hard for you, so treat it well.
Keep the Conversation Going
- Visit our blog for more women’s health tips.
- Join our private Happy V Facebook group to hear from others who've been there.
- Explore supplements designed to support your vaginal health journey.
Disclaimer: This blog is for informational and educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Statements about supplements have not been evaluated by the Food and Drug Administration. For more information about vaginal infections, visit the CDC or speak to a licensed healthcare provider.